The condition of “Low T” is running rampant all over the media these days and there has been a huge increase in testosterone prescriptions[1], especially in the US, likely due to direct to consumer marketing but also confounded by incomplete workups and premature treatment. There is also much interest in optimizing or raising testosterone both in the fitness and general health/wellness communities even though the evidence suggests that having “high testosterone” and “low estrogen,” etc is not necessarily optimal for overall health[2] while quality of life scores more closely correlate with obesity in elderly men.[3] Spencer’s blog accompanying this touches on that misconception regarding the desire for needing high levels of endogenous testosterone while we absolutely do NOT condone using exogenous testosterone (steroids) or other hormones at supraphysiologic levels which obviously give a physical edge but have significant adverse health effects and are considered cheating in sports (for what it is worth, we hope to set examples of healthy physiques built without use of steroids).
I wanted to touch on the subject of low testosterone in the setting of obesity, specifically abdominal obesity. I’m not referring to the “andropause” (which is actually a misnomer and correlates more to the term “Late Onset Hypogonadism[4]” which has a pattern of primary testicular failure[5] as we age) but to the complex dysfunction of the hypothalamic-pituitary-testicular axis which is part of the vicious cycle of abdominal obesity and potentially metabolic syndrome, diabetes, and heart disease.
A couple of months ago, I presented a grand rounds to my endocrinology colleagues regarding the topic, so I’ll try to boil it down to a more patient-friendly version with recommendations.
First of all, if you think you have symptoms (low libido/energy, muscle loss, decreased hair growth, etc) then a discussion with your physician is warranted along with a thorough evaluation[6] to diagnose the underlying disorder, and if truly “low T,” then continued evaluation to find the underlying cause. The last thing people should do is ask for treatment without knowing why a hormone is low or dysfunctional.
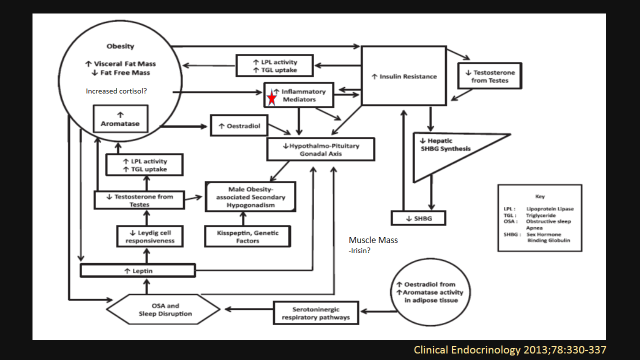
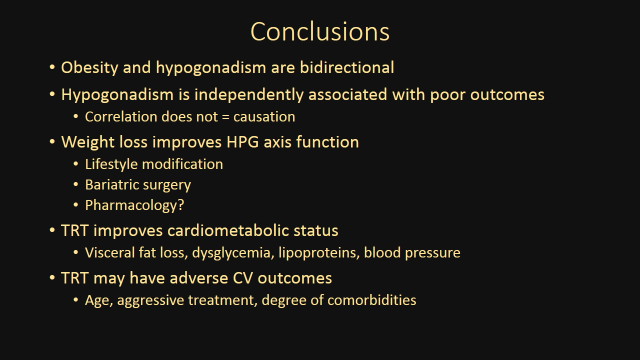
You may be aware that obesity is a very complex disease involving genetics, environment, diet, physical activity, sleep, and the complex interactions between our adipose (fat) tissue, muscles, and other endocrine (hormone) organs with our brain (hypothalamus) and back to our endocrine organs. This includes a vicious cycle of secondary hypogonadism[7] (the hormones from the pituitary are inappropriately low for the low testosterone from the testicles). I call the association of low testosterone with abdominal obesity[8] and metabolic syndrome[9] and diabetes[10] “bidirectional” because the obesity causes dysfunction to the testosterone axis while low testosterone certainly does not help[11] the pathology of obesity in males. Low testosterone has also been associated with increased overall death[12] and death from heart disease (coronary artery disease)[13] in meta-analysis but correlation does not equal causation and very low testosterone is a good marker of poor health predicting death[14] while higher levels may predict reduced cardiovascular event risk.[15] This has lead to the proposal of a diagnosis focusing on male obesity-associated secondary hypogonadism or MOSH[16] defined as BMI > 30kg/m2 (I would argue that waist circumference would be better), signs/symptoms (sexual/physical/mental disturbance, gynecomastia, sleep disturbance, abnormal glucose homeostasis, low bone mass, or unexplained anemia, etc), total testosterone lower than lower limit for young healthy men confirmed twice (which is about < 350ng/Dl and free testosterone should be used for most patients with obesity due to lower sex-hormone binding globulin), and low or inappropriately low luteinizing hormone & follicular stimulating hormone while ALL OTHER CAUSES ARE EXCLUDED.
Obviously it seems reasonable, then, that if your belly fat is causing low testosterone and low testosterone is associated with the other bad things associated with belly fat, then we should replace the testosterone right? Well that is very debatable these days based upon the available evidence. I’ll take this time to again remind everyone that if their testosterone is truly low, then a thorough evaluation needs to take place to diagnose the true underlying cause before treating it as “MOSH.” There certainly is evidence that testosterone replacement therapy helps lose weight[17] along with improvements in cardiometabolic risk parameters including diabetes[18]. There are other pharmaceutical methods we utilize in endocrinology to help increase the body’s own endogenous testosterone production which I am very interested in but is beyond the scope of this article and the supplements promoted for increasing testosterone are either dangerous or not very efficacious, consider checking out examine.com for more info on that. So what to do? Well first, do no harm.
Unless you don’t watch TV or get news on the internet, due to the media, that there has recently emerged a growing concern about the adverse cardiovascular events which may accompany using testosterone replacement therapy in older men with higher risk of heart disease leading the Endocrine Society to issue a statement of caution (I contributed to that!). Other than one recent study showing reduced mortality[19] (death) and an observational study associating reduced mortality with treatment, a meta-analysis last year[20] plus two recent studies (the VA study on men who underwent coronary angiography[21] and the large cohort comparing those prescribed testosterone vice erectile dysfunction meds[22]) revealed increased risk of heart attacks and deaths. Now these are certainly not studies elaborate enough to give us the answer we all desire, but enough to prescribe cautiously and really weigh the benefits versus potential risks.
So what to do? Well this is the part where we get back to a Leaner Living lifestyle. It is well established that doing what needs to be done to lose that belly fat will increase testosterone[23] regardless of diet, exercise, or (most dramatically) bariatric surgery and weight maintenance sustains the increased testosterone[24]. Caloric restriction helps on its own,[25] while increased exercise volume[26] and resistance training[27] garner benefit and as always, the unsung here, sleep optimization (including evaluation for, and treatment of, obstructive sleep apnea).
So when discussing this with your physician, I would avoid looking for testosterone replacement, and instead work hard to enhance your diet, exercise, and sleep as I emphasize with all my patients and work closely with your physician (possibly an endocrinologist) to consider the all the treatment options while weighing the risks/benefits of all.
[1] J Clin Endocrinol Metab 2014;99:835-842
[2] J Clin Endocrinol Metab doi:10.1210/jc.2013-3272
[3] Age Ageing 2014;43(2): 280-284.
[4] N Engl J Med 2010;363:123-35
[5] J Clin Endocrinol Metab 2010;95:1810-1818
[6] J Clin Endocrinol Metb 2010;95(6):2536-59
[7] Clinical Endocrinology 2013;78:330-337
[8] Curr opin Endocrinol Diabetes Obes 2013;20:132-139
[9] Int J Epidemiol 2011;40(1):189-207
[10] Eur J Endocrinol 2010;162(4):747-54
[11] J Natl Cancer Inst 2010;102:39-46
[12] J Clin Endocrinol Metab 201;96(10):3007-19
[13] Heart 2011;97(11):870-5
[14] J Clin Endocrinol Metab doi:10.1210/jc.2013-2052
[15] J Am Coll Cardiol 2011;58:1674-1681
[16] Clinical Endocrinology 2013;78:330-337
[17] Obesity (Silver Spring) 2013;21(10):1975-81
[18] Diabetes Care 2011;34:828–837
[19] Eur J Endocrinol 2013;169(6):725-33
[20] BMC Med 2013;doi: 10.1186/1741-7015-11-108
[21] JAMA 2013;310(17):1829-1836
[22] PLoSONE 2014;9(1):e85805
[23] Eur J Endocrinol 2013;168(6):829-43
[24] Diabetes Obes Metab 2004;6(3):208-15
[25] Horm Metab Res 2013
[26] J Sex Med 2013;10(7):1823-32
[27] J Applied Physio 1999;87(3):982-992